Penicillin Hypersensitivity
Download / Print Section as PDFPenicillin Hypersensitivity
-
The risk of penicillin hypersensitivity is an important one, as anaphylaxis can be fatal. On the other hand, avoidance of penicillin because of concerns regarding allergy is widespread, and in many situations unnecessary.This leads to increased use of broad-spectrum antimicrobials which contributes to development of antimicrobial resistance, and is associated with higher morbidity and mortality in these patients (e.g. suboptimal therapy, C. difficile infection), longer hospital stay and higher healthcare costs.
-
An accurate patient history is important when evaluating allergy. Important details of an allergic reaction include signs, symptoms, severity, timing of onset of the reaction in relation to drug exposure, antimicrobial agent and administration route used, date of event, prior reactions, subsequent exposure to same or related agents, other medicines being taken concurrently, time and route of their administration, and adverse drug reactions to other medicines.
-
Record allergies carefully in the medical notes and on the drug chart including date of reaction and your signature and MCRN.
-
Transfer allergy information when re-writing the drug chart.
-
Check with the patient and the allergy section of the drug chart prior to prescribing and administering all antibiotics.
-
-
Assess reported symptoms critically to exclude non-allergic adverse reactions (e.g. diarrhoea, vomiting, non-specific maculopapular rash) or reactions wrongly attributed to the antibiotic (e.g. treatment with amoxicillin is associated with rash in 80% of patients during Epstein-Barr virus infection). Do not document these as “allergies”. If in doubt, consider consulting Immunology.
-
-
For the purposes of prescribing in penicillin allergy it is important to differentiate between an immediate hypersensitivity reaction, a severe delayed hypersensitivity reaction and a non-severe delayed hypersensitivity reaction. Relevant definitions are:
-
Immediate - occurring within one hour of drug administration
-
Delayed - occurring more than one hour after drug administration
-
A minority of patients with a delayed hypersensitivity reaction will have a history of severe delayed hypersensitivity reaction (e.g. Stevens-Johnson Syndrome (SJS), Toxic Epidermal Necrolysis (TEN), Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), and Acute Generalised Exantematous Pustulosis (AGEP)).
-
-
Patients with a history of immediate (within one hour) hypersensitivity reaction (anaphylaxis, laryngeal oedema, bronchospasm, hypotension, local swelling, urticaria or pruritic rash ) should not receive a penicillin, cephalosporin or carbapenem (e.g. meropenem) . If there is a compelling reason to consider the use of a beta-lactam agent in such a patient consult Microbiology or Infectious Diseases, and contact the Department of Immunology who may be able to assist in assessing if the patient is likely to be hypersensitive to all beta-lactams.
-
Patients with a history of severe delayed hypersensitivity reaction (SJS, TEN, DRESS, AGEP) to penicillin should not receive any beta-lactam – consultation with Immunology/Dermatology advised.
-
Patients with a history of a non-severe rash with a delayed onset of more than one hour after penicillin administration may reasonably be prescribed a cephalosporin or carbapenem.
-
Patients for whom little or no information is available (after making every effort to determine allergy history), should not receive penicillin in the first instance but may be prescribed a cephalosporin or carbapenem with caution . Consider referral to Immunology for further investigations.
-
Aztreonam can be used in patients with allergy to penicillin, but consider with caution in patients who are allergic to cefTAZIDime due to similar side-chain.
-
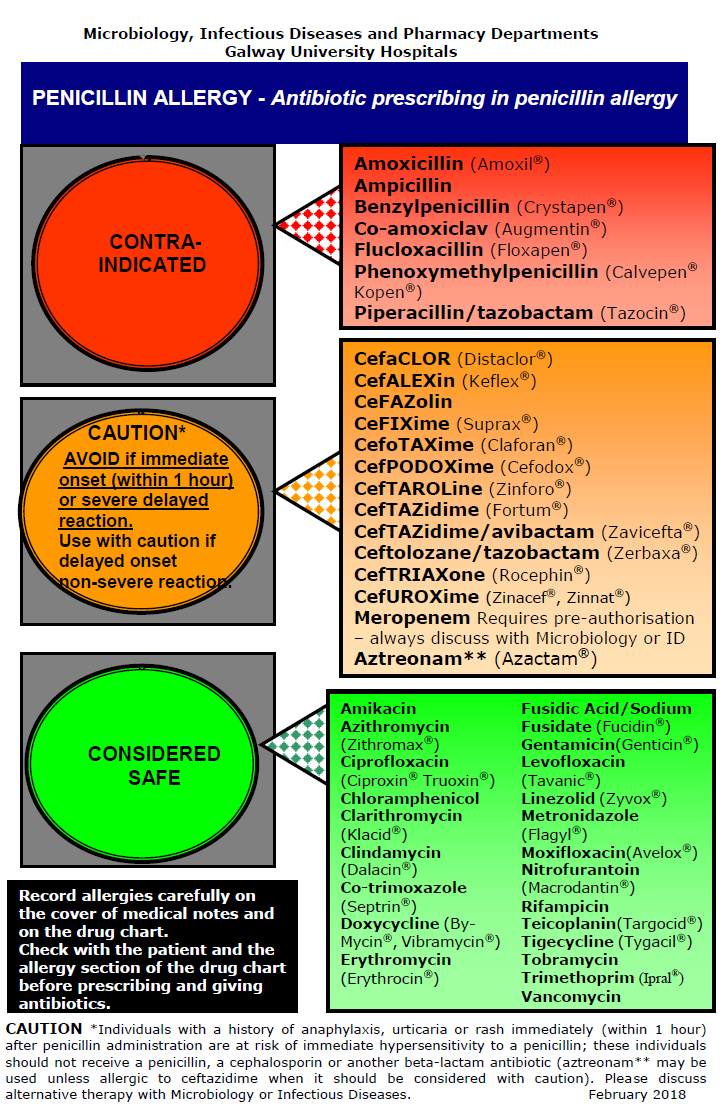
The Penicillin Allergy Traffic Light Poster lists antibiotics that are contraindicated, can be used with caution and are considered safe to use in penicillin allergy.
-
Refer people with a suspected allergy to beta-lactam antibiotics to Immunology if they
a) need treatment for a condition that can only be treated by a beta-lactam antibiotic or
b) are likely to need beta-lactam antibiotics frequently in the future (e.g. those with anatomical predisposition to infections or immunodeficiency).
Refs:
- Demoly et al. International Consensus on drug allergy. Allergy 2014 (69) 420-437
- Shenoy et al. Evaluation and management of penicillin allergy. JAMA 2019;321(2):188-199.
- www.antibioticprescribing.ie
- Drug allergy: diagnosis and managements. NICE clinical guidelines 2014. https://www.nice.org.uk/guidance/cg183 (Reviewed in 2018)